As we envision data stewardship as a means to unlock public benefit from data while preserving data rights and meaningfully engaging communities – scalability becomes a matter of concern. This is because stewards largely rely on external revenue streams due to ethical concerns on monetising sensitive health data and hence struggle to achieve scale. Meanwhile large pharma companies devise arrangements for collecting and sharing of health data that are in conflict with data privacy rights. This play lays down strategies to provide pathways to secure and ethical data sharing with private stakeholders and to diversify revenue streams and provide models that enable scaling of stewarding initiatives while providing public benefit.

Challenge h3.1
Lack of well-seated funding interests and revenue models
With ethical and legal conundrums on the ability to monetize sensitive health data, stewards in this sector rely on external revenue streams of limited government grants or philanthropic donations, which are competitive and uncertain to achieve scale. Private industry partners such as pharmaceutical companies, insurance agencies, and medical device manufacturers may also be invested in funding research and data collection initiatives. However,the underlying market-driven logic that motivates such efforts raise ethical questions about affordability, democratic access and patient autonomy. Practices of large pharmaceutical companies like Pfizer and the role of philanthropies like Bill & Melinda Gates Foundation on the procurement and distribution of Ebola virus or COVID-19 vaccines, for instance, exacerbated health inequities in times of crisis. Similarly, arrangements for collecting, analysing, and sharing medical records as devised by large data brokers such as the IMS Health have been documented to go in conflict with the data privacy rights. These electronic records are collected from a variety of sources including pharmacies, insurance companies, and public health departments, yet fall outside the purview of privacy regulations by virtue of being anonymised – drawing attention to a glaring lacuna in prevailing data regulation regimes. Focusing on internal revenue streams of subscription or service fees, advertisements, or monetizing patient data, on the other hand, risks diminishing the pluralistic value inherent to data exchange. Stewards then assume the role of brokers concerned with monetisation alone, as opposed to facilitating meaningful collective bargaining around data rights as envisaged by scholars.


Strategy h3.1.1
Diversifying revenue streams and adopting cost effective models
Considering the high costs associated with managing health data, and extracting value for the sector, health data stewards must build a balanced model of generating revenue for sustenance through both internal and external revenue streams. The Rhode Island Health Information Exchange has developed a business model based on contributions from both the public and private sectors to build consent based access to patient health information for private healthcare providers as well as users and public health departments. Similarly, models such as that of MiData have tapped into the potential of effectively utilising internal revenue generation mechanisms such as membership or subscription fees, that go alongside external grants, by incentivising users with secure storage of and control over their data.
As recognition of the value of health data stewardship models increase, new models and grants are being introduced to support stewarding initiatives that operate ethically and bring benefit to the community. The Learning and Action in Policy and Partnerships (LAPP) program led by Data Across Sectors for Health (DASH), for instance, has come up with grants to promote collaborations for community data exchange that attempts to bridge multi-sector data from states and communities towards achieving health equity for specific target groups. Similarly, the eHealth Exchange, a non-profit health information network that connects providers and federal agencies, has announced grants for technical innovations that promote interoperability for health information exchange.



Strategy h3.1.2
Build appropriate safeguards to make space for secure private sector data sharing and showcase value of health data exchanges within ethical frameworks

While there are various concerns that have been highlighted in challenge 1 for this play on funding and health data sharing with pharmaceutical companies, medical device manufacturers, and insurance companies, our research has found that in the long-term, private sector stewardship initiatives tend to be more sustainable than entities funded by the government. Accordingly, through the adoption of appropriate legal and technical safeguards that address the ethics of data sharing with such private stakeholders, we can help projects scale while maintaining community benefit. Towards this, on the one hand we need sectoral regulation such as Health Insurance Portability and Accountability Act of (HIPAA) and Personal Health Information Protection Act (PHIPA) to protect the privacy of the individuals through de-identification, consent mechanisms, and purpose limitation etc., and govern data sharing agreements that clearly outline the terms and conditions of the data sharing. Additionally, there must also be standards on data sharing, transparency, and governance processes, such as the HL7 Fast Healthcare Interoperability Resource (FHIR), that unify definitions, and promote data quality checks.
The model adopted by the UK Biobank provides a helpful case study on the nuances to private sector data sharing by large scale data stewards. Their model operates as a large-scale, long-term health study that collects and stores volunteered health data. Partnerships between the UK Biobank and pharmaceuticals like Astrazeneca on data access for drug research operates through de-identified volunteer data contributions to drive insights that are then made available to the global scientific community. However, the Biobank model has been criticised on data-privacy and ethical concerns, and for lacking scientific value owing to its limited data points that lack diversity and community participation. Alternate models, such as that of the All of Us Research Program in the USA and Saluscoop data cooperative, have been hailed for successfully addressing the challenges around diverse datasets and citizen participation for health data governance respectively.
Challenge 3.2
Low realisation on incentives, trust, and capacities for individuals and other stakeholders
Over the past few years, models for data stewardship have been conceptualised in various forms such as data trusts, data collaboratives and data cooperatives across geographies and sectors. However, meaningful adoption of these initiatives are still largely hinged on limited citizen data contributions and engagement, sporadic funding and other technical barriers. To scale stewarding initiatives, , there is a need to ensure consistent and widespread participation from individuals and communities, while building a collaborative ecosystem for funding and interoperability.
However, the road to building this ecosystem lies in addressing deeper socio-cultural complexities that impede active citizen engagement and healthy partnerships to build equitable health data futures. Historically, unethical health research practices aimed at profiling or surveillance have inculcated a deep seated suspicion on sharing health data for public research purposes. Events such as the Tuskegee Study, and the Guatemalan STD Study for instance, collected the data of unsuspecting black populations, prison inmates, mental patients, and soldiers under the garb of providing treatment for syphilis. In the modern context, the public attitude on sharing sensitive personal health data with large corporations remains sceptical as a result of exploitative use within insurance and pharmaceutical industries, as well as broken data governance structures. To successfully undertake public research and community-driven biomedical initiatives, concerted efforts must be undertaken that involve transparent practices that prioritise public value, as opposed to merely surfacing monetary incentive. Research has pointed to the complications in paying individual people for their health data which could deepen the economic inequities and fail to counter the power asymmetries that pit individuals as inherently disempowered in relation to public bodies and companies.
The ideal ecosystem for health data stewardship to thrive also involves an open and collaborative space to access and exchange data, insights, and associated services. At this stage, behemoths such as the IMS Health undertake the high costs of collecting and maintaining complex health data which otherwise remains siloed within different organisations. Additionally, there is a general lack of standardisation on the taxonomy for health data rights, use, and sharing, and a dearth of adequate level of interoperability within the healthcare system. This isolates the different service providers, researchers, and the public healthcare system, and deprives the ecosystem of the cost and labour benefits of a secure unified system

Strategy g3.2.1
Identify, build, and communicate health data value to people, society, and stakeholders to incentivise citizen engagement

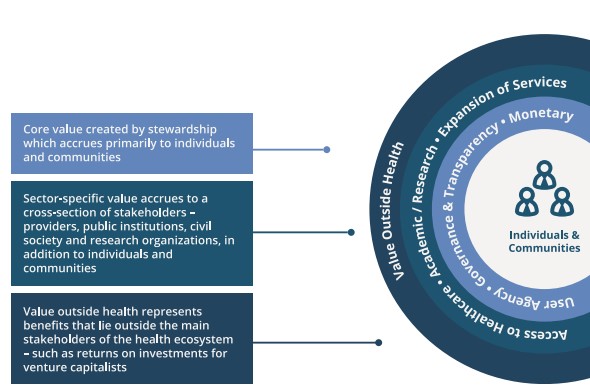
Higher citizen engagement throughout the data life cycle is crucial to scaling a health data stewardship model. Community participation in the data collection and governance processes can be incentivised by appropriately identifying and communicating health data value and the benefits of active participation to specific target groups. In our work, we have articulated the value created by health data stewardship as disaggregated into three categories – core values such as user agency and accountability, sector-specific values around drug research or expansion of access to healthcare providers, and external values like revenue generated for investors and stakeholders outside the healthcare ecosystem.
Research has also found that these incentives can differ for people based on how they prioritise public benefit against the involvement of private bodies in controlling their health data, their understanding of the data rights and associated risks, and their experiences and faith in the system. As a secure and reliable governance structure is put in place to ensure privacy rights, a variety of public benefit manifestations can be communicated with the people to sway their willingness to engage with health data initiatives. These can range from the potential of developing a life-saving drug, sophistication in treatments and diagnosis for illnesses, and greater access to services for vulnerable groups, to ease in accessing or repeating prescriptions and improved agency and responsiveness of services and health data corrections.
Health data value can be made visible through the adoption of models such as the Bermuda Principles of Genomic Data around the Human Genome Project which promotes rapid and free public release of pre-published DNA sequence data among scientists. During the COVID-19 pandemic, the project played an important role in facilitating insights to the disease and displayed how health research endeavours can work towards the common benefit of all people. Critiques have surfaced on the efficiency of data sharing and access to similar models, however there is consensus on the value of enforcing such principles as a standard practice. and potential which makes the investments in their constant improvement worthy.
More direct strategies on actively identifying and communicating data value to people are also being adopted elsewhere, with projects such as the Data Saves Lives Toolkit and the Toolkit for Communities Using Health Data by National Committee on Vital Statistics. These efforts aim to support better dialogue with communities on their health data and to enable patient groups to potentially launch their own health data initiatives. This takes a step-wise approach on explaining how data can advance health outcomes, explains the various health data tools involved, provides communication strategies and patient surveys, and assists with risk assessments that together help match the differing priorities of communities.



Strategy g3.2.2
Build technical capacities and promote collaborations within industry
Considering the highly technical nature of health data management, scaling can be made efficient by leveraging partnerships between public health institutions, technology firms, and healthcare providers for resource sharing within existing data stewardship programs, and with other organisations that share similar goals.
Models such as theYale University Open Data Access (YODA) Project have institutionalised collaboration by encouraging sharing of clinical research data across government, academia, and private players, thus facilitating meta-analyses, replication of results from trials, and building research on prior findings. In the UK, the NHS England acknowledged the value of partnerships in this space and built a report on the foundations of fairness for NHS health data partnerships which provides a clear guiding point on collaborations and involves the public in conversations on good data governance and trustworthy health data systems.
Their research aims to promote transparency and public access to the partnerships in this space, emphasise on the importance of equity in measuring their impact, and enabling an open environment on local NHS partnerships that is conducive to negotiating fair terms amongst themselves and third parties.
Beyond sharing data and insights through partnerships, it is also crucial to encode privacy and data rights to build trust towards the creation of a collaborative ecosystem. Sector specific regulations such as USA’s HIPAA and Patient Safety and Quality Improvement Act (PSQIA) as well as the PHIPA in Ontario, Canada address the specific concerns on health data rights and enforce standards like HL7 FHIR for health data sharing. Apart from regulations, initiatives such as Redox provide essential case studies on stewards themselves building trust in the ecosystem through their model on creating a unified protocol for electronic health records maintenance that can be used as standards for data exchange between providers, insurers, and patients all under one framework.
